This is the second in a series of articles on Quality Culture in the Medical Device Industry. For the first article in the series, click here.
In today’s competitive business landscape, the significance of a robust quality culture cannot be overstated. As François Sallans of Johnson & Johnson aptly noted, “The degree to which quality is embedded in an organization’s culture can mean the difference between success and failure.” This sentiment is echoed across industries and regulatory bodies, highlighting the critical role of quality culture in achieving long-term success.
This post explores why cultivating a robust quality culture is essential for business success and how organizations can overcome the challenges of establishing and maintaining it.
Table of Contents
Signs of a Weak Culture of Quality
Understanding the symptoms of a weak quality culture is the first step towards improvement. Forbes Insights, in partnership with ASQ, has identified some key warning signs that an organization’s quality culture may be lacking:
Lack of Executive Engagement: The CEO and senior executives rarely discuss quality or performance against quality objectives.
Quality is not routinely included in leadership team or management board agendas. Management Reviews are not conducted with sufficient frequency that the senior and executive leaders have a robust understanding of the quality and compliance risks and the consequences of a lack of poor quality and inadequate compliance with regulations.
Disconnected Quality Vision: The company’s vision is either non-existent or weakly linked to business strategy and company vision and/or mission.
Employees are either unfamiliar with or view the quality policy or stated quality value(s) as mere slogans or wall decorations. New employees are not oriented to the company’s policy and culture regarding quality.
Managerial Resistance: Managers either fail to emphasize quality consistently or resist quality initiatives.
As new regulations are established by FDA and other global health authorities, does management embrace and enable the change or resist it? Company Senior Leadership Teams and Executives drive to achieve on-time product launch to achieve strategic business and financial goals. Do they place the same emphasis or focus on the quality of the medical device design and manufacturing process(es)?
Neglect of Product Quality Complaints and Adverse Events: No formal mechanisms exist for collecting and analyzing product quality complaints, device malfunctions, and adverse events.
This, combined with a lack of a valid statistically based methodology to trend product quality complaints/device malfunctions to identify the need for corrective and/or preventative action is a critical warning sign of poor quality culture.
Inadequate Quality Performance Management Measures in Employee Goals and Objectives: Quality goals are not reflected in performance evaluations for employees in all functions and all levels within the organization.
Research and Engineering teams are rewarded for on-time launch of new medical devices; they are not rewarded for device designs that yield high-quality products with very low risk of failure or malfunction. Manufacturing teams are rewarded for case fill rate or unit fill rate and on-time delivery to customers. When FDA issues a 483 or Warning Letter to a device manufacturer, it is often the VP or Head of Quality who is seen as the “poor performer”. The heads of the other functions are not held accountable or are not held accountable to the same degree.
Frequent Product Supply Interruptions and Delays due to Product Non-Conformances at Supplier Sites or Primary Manufacturing Sites.
Delays in New Product Approvals/Launches due to Product Design or Manufacturing Issues. Frequent Non-Conformances and/or Rejections due to inconsistent quality or quality failures. A high level of “concessions” or “accept as is” approvals due to substandard quality.
Do any of these symptoms of poor quality culture seem familiar to your company?
The Cost of Poor Quality
The financial implications of poor quality culture are significant. Poor quality culture often leads to increased nonconformances, device malfunctions, device failures, adverse events, and regulatory observations, such as 483’s, or warning letters. The costs associated with a major deviation or FDA 483 observation can be staggering and are often underestimated.
Operational excellence is now the foundation of high-performing medical device companies. McKinsey underlines this point in a recent MedTech Pulse report: “As companies grow bigger and devices become more complex, operations will be a differentiating factor for MedTech leaders. MedTech companies can improve their operations to become more reliable, robust, and profitable, ultimately delivering better patient care.” To be have reliable product supply and robust product performance an organization must have a robust quality culture at its foundation.
The problem is, many medical device companies are far from achieving operational excellence. One only needs to review the list of medical device recalls on the FDA website from 2023 and 2024YTD to see the issues related to poor product design and/or manufacturing.
The cost of a recall or correction can easily cost in excess of two to five million dollars or much more depending upon the number of devices recalled. This does not include the impact to patient care due to unavailability of the devices subject to recall. Once again, the organization must have a robust quality culture driven from the top of the organization down through and across the entire organization to prevent the launch of medical devices with design flaws and/or suboptimal manufacturing processes.
Direct Costs
Hundreds of thousands to millions of dollars are spent on root cause investigations, CAPA planning and execution, rejected products, and documentation revisions. The cost of a CAPA to correct medical device design deficiencies can easily cost one to three million dollars or more.
Potential Additional Costs
Including costs for external experts and consultants, recalls, process improvements, and follow-up correspondence with FDA, can easily exceed $2 million.
The average small quality and compliance remediation project generally costs 3 to 7 million dollars. The cost of large, complex quality and compliance remediation projects can run from 10 million dollars to over a hundred million dollars.
History of FDA’s Increasing Focus on a Robust Quality Culture
As part of its Vision for the 21st Century, the FDA has progressively emphasized the importance of a robust quality culture. Innovations such as Design Control, introduced in the mid-1990s reflect this shift when the QSR was implemented. The FDA’s inspection approach now includes evaluating the maturity of an organization’s quality culture, emphasizing commitment to quality throughout the product lifecycle.
FDA has presented a number of times on the topic of quality culture over the past 5 to 8 years. This slide has appeared in most of those presentations made by FDA:
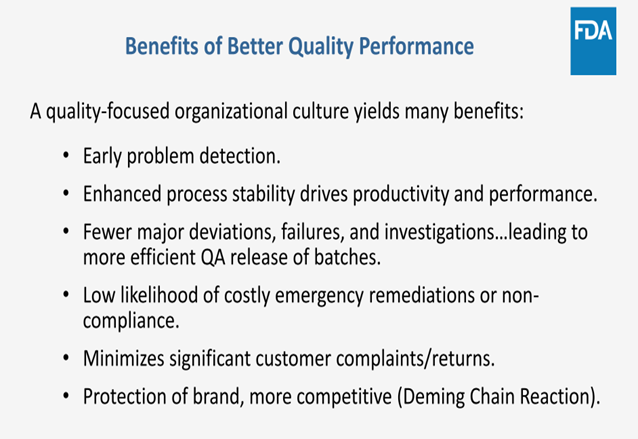
FDA has clearly identified the correlation between poor quality culture, product quality issues, and less than optimal compliance with FDA regulations.
Two Critical to Quality Elements in Establishing a Robust Quality Culture
Creating a robust quality culture is easier said than done. It requires more than just slogans and policies; it demands deep integration into every aspect of the organization. To build a lasting quality culture, it’s essential to change the context in which employees operate. To accomplish that you need a good diagnosis. One that starts at the top of the organization and obtains feedback at all levels throughout the organization.
Holistic Approach
The challenge lies in embedding quality into the corporate psyche, ensuring it consistently influences people, processes, products, and services.
Quality must be a peer-driven initiative supported by the top levels of management and integrated across all functions.
Organizations must go beyond compliance to regularly assess and improve their quality culture using data-driven insights. A focus on compliance with regulations will not enable high quality product design, manufacturing processes, and end user experiences.
Diagnosing the Quality Culture with the Right Diagnostic Tool
There are many quality culture surveys available, but most focus on the QMS itself and not on the observed behaviors and perceived values and norms held within the organization about quality.
Culture is based upon values and beliefs and is expressed through behaviors.
Quality Culture surveys focused on the number of late CAPAs, and Deviation Investigations or other quality metrics provide information on the results of a poor quality culture. They do not help you understand the values and norms which shape the culture. They do not help you understand what must be enhanced within, added to, or edited out of the organization’s beliefs, norms and values to realize and sustain a high value for quality.
To measure Quality Culture, organizations must select a tool that characterizes the observed behaviors regarding all aspects of quality to gain valuable insights into the norms and values of the company. Simply looking at the number of late CAPAs, nonconformances, and product quality complaints is not sufficient. Once a baseline is established, the tool should be used at appropriate intervals to monitor progress of the actions executed to improve quality culture.
Conclusion
Aristotle once said, “Quality is not an act; it’s a habit.” Companies must weave quality into the fabric of their organization instead of treating it like a one-off project or corporate initiative.
Achieving and maintaining a robust quality culture is not just a compliance exercise but a strategic necessity. Organizations that embed quality into their culture see significant benefits, including reduced deviations, lower costs of quality failures, and enhanced regulatory compliance.
Contact Us
To learn more about importance of creating a robust quality culture and Compliance Architects’ propriety tool for assessing quality culture, please fill out the form below to contact us.





